Needle stick injury protocol pdf
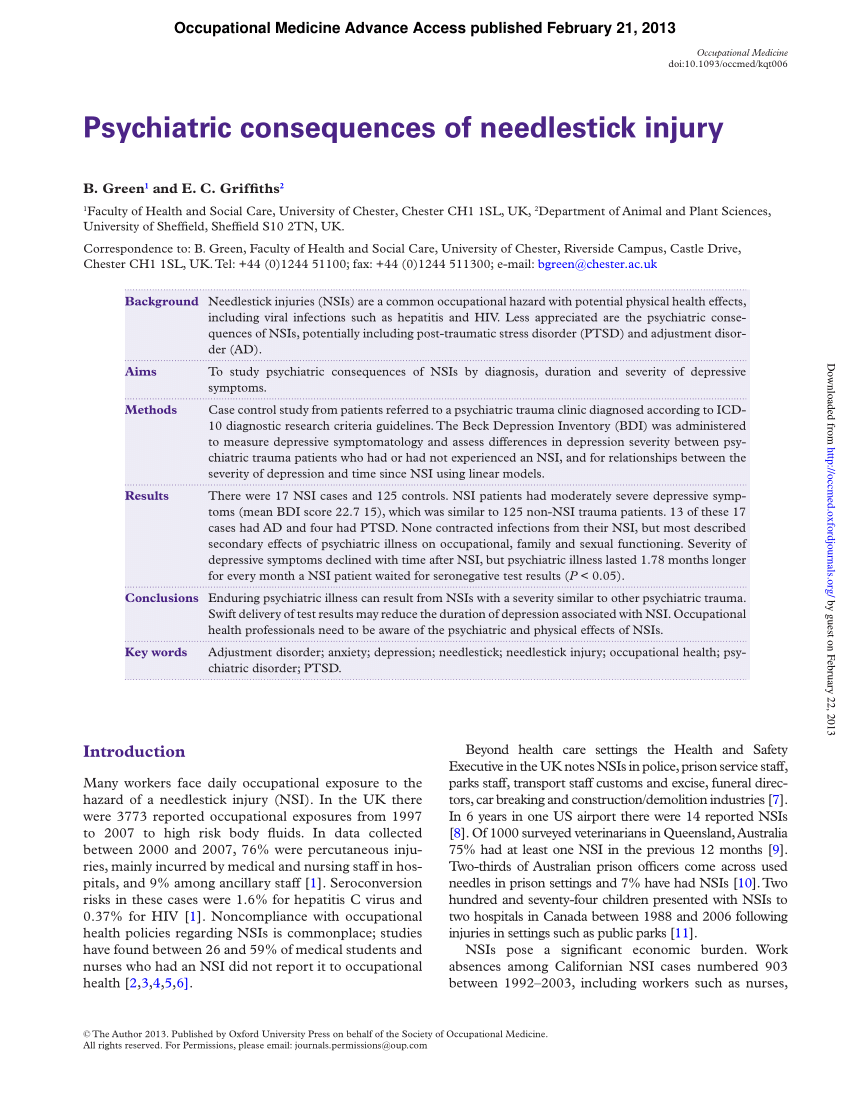
1 Recommendations on the Management and Postexposure Prophylaxis of Needlestick Injury or Mucosal Contact to HBV, HCV and HIV Background Occupational exposure …
In this section. Australian National Guidelines for the Management of Healthcare Workers Living with Blood Borne Viruses and Healthcare Workers who Perform Exposure Prone Procedures at Risk of Exposure to Blood Borne Viruses
“Needlestick and other sharps injuries are a serious hazard in any healthcare setting. Contact with contaminated needles, scalpels, broken glass, and other sharps may expose healthcare workers to blood that contains pathogens which pose a grave, potentially lethal risk.
Needlestick injuries are a potential risk to health professionals who use needles and syringes in their clinical work. The New Zealand Health Strategy includes a framework and action plan to reduce the incidence and impact of infectious disease in an occupational setting. 1 Needlestick prevention protocols are an important element of the action
A needlestick injury, percutaneous injury, or percutaneous exposure incident or sharps injury is the penetration of the skin by a needle or other sharp object, which has been in contact with blood, tissue or other body fluids before the exposure.
Needlestick Injury: the accidental puncture of the skin by a needle during a medical intervention. Accidental exposure to blood: the unintended contact with blood and or with body fluids mixed with blood during a medical intervention.
from a Needle Stick Needle stick injuries pose a risk if the needle is contaminated with Hepatitis B, Hepatitis C or HIV virus. The risk of contracting an occupational disease caused by a needle stick depends on a number of factors: • the depth of penetration of the needle, • the amount of contaminated blood on the needle • when the needle was used, • the health status of the infected
A needlestick injury means the skin is accidentally punctured by a used needle. Diseases that could be transmitted by a needle or needlestick injury include human immunodeficiency virus …
needle stick injuries, its awareness, frequency of injury and the protocols that were followed after an injury had occurred. These questionnaires were given to 500 health care workers working in different wards and theaters of the hospital after
NEEDLE STICK INJURIES Sharps injuries are the most frequent occupational hazard faced by nurses, phlebotomists, doctors and other healthcare workers1.
Needlestick Injuries in Dentistry KUMJ
Needlestick Protocol WHAT TO DO Occupy Medical
Needle-stick injuries in members of the public A major source of distress is the needle-stick injury sustained by members of the community – usually from syringe/needle combinations that have been discarded in a public place.
needlestick injuries. LLÞtgog Queensland Health Centre for Healthcare Related Infection Surveillance and Prevention rnl/cc . Title: Poster: Protect Yourself and Others Author: CHRISP Subject: Five simple steps to avoid needlestick injuries Keywords: poster, needlestick injury, avoid needlestick Created Date : 8/9/2010 1:10:57 PM
The purpose of this report is to present the infection control protocol for needlestick and similar sharps injuries for approval. the protocol is attached
The purpose of this report is to present the Infection Control Protocol for Needlestick and Similar Sharps Injuries for approval. The Protocol is attached
Needlestick Injury – from the community Page 2 of 4 Emergency Department Guideline Calculated from column 1 and 2. Maximal risk is likely overestimated.
needlestick and other occupational injuries, especially in the light of recent legislative change (Human Tissue Act 2004 [HTA] and Mental Capacity Act 2005 [MCA]), and the withdrawal of previous guidance from the General Medical Council (GMC).
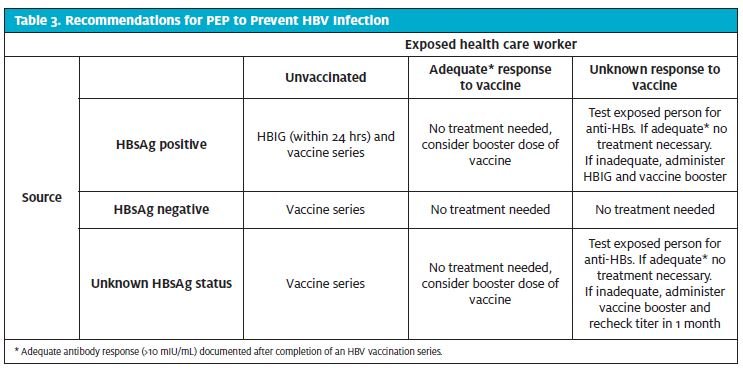
An occupational exposure by an employee is defined as a needle stick, sharp puncture wound or a splash to mucous membranes (i.e., mouth or eye) with blood or body fluids as a result of an assignment at an affiliated hospital.
The AIDS Institute’s Office of the Medical Director needlestick injury procedure is as follows: If there is a needlestick injury and assistance is needed from the AIDS Institute,
ODNS 2015 89 43. Guidelines on Needle stick Injury The following information is abstracted from the South African Department of Health guidelines entitled:
Management of community needle stick injury (CNSI): Presentations of children to Emergency Departments following accidental needle stick injury are not uncommon and such injuries may be a significant source of anxiety.
Needle-stick injury (NSI) is a major occupational health and safety issue faced by healthcare professionals globally. This study was aimed to assess the frequency and factors associated with NSIs
Clearly, the appropriate management of needlestick injuries poses a new challenge to the healthcare sector, both in terms of reducing the overall risk of needlestick injury, the fair and reasonable management of injured staff and the protection of patients.
•the safety feature cannot be deactivated and remains protective through disposal Workplace Protocol •Use the devices with safety fea-tures provided by the employer.
Needlestick and sharps injuries are recognised as one of the significant occupational hazards faced by healthcare workers every day. Every needlestick or sharps injury carries the risk of acquiring a potentially life threatening bloodborne disease such as hepatitis B or C, or HIV/AIDS.
NEEDLESTICK INJURIES POLICY Policy for the procedures to follow in the event of staff and students who have been exposed to blood and blood stained body fluids in the course of carrying out their duties.
Here are some other needlestick resources from www.drotterholt.com. [Editor’s note: Visit Dentaltown.com to view these links.] Post-Exposure Prophylaxis Hotline (PEPline) is a national toll-free hotline (24 hours a day)
A needlestick injury means the skin is accidentally punctured by a used needle. Diseases that could be transmitted by a needle or needlestick injury include human immunodeficiency virus (HIV), hepatitis B and hepatitis C.
precaution guidelines and Malaysia infection control guidelines with objectives to promote the students interests on the universal precaution measures on needle sticks injury and to prevent future transmission of infection through needle stick injuries. So we had set the objectives for the research to study the effectiveness of Needle stick injury prevention intervention model on accidental
A needlestick or sharps injury is said to have occurred if a staff member punctures the skin with a needle or sharp instrument that has been in contact with a patient’s blood. Splashing of the conjunctiva with blood or other body fluids is also included.

This guideline pertains to needlestick injuries from discarded needles in the community, usually from an unknown source where the risks of blood-borne virus (BBV) transmission, i.e. Hepatitis B, Hepatitis C and HIV, are very low.
for 63% of the needlestick injuries from June 1995 July 1999 (NIOSH, 1999). Ninety percent of the Centers for Disease Control and Prevention (CDC) document- ed cases of health care workers who contracted HIV from needlestick injuries
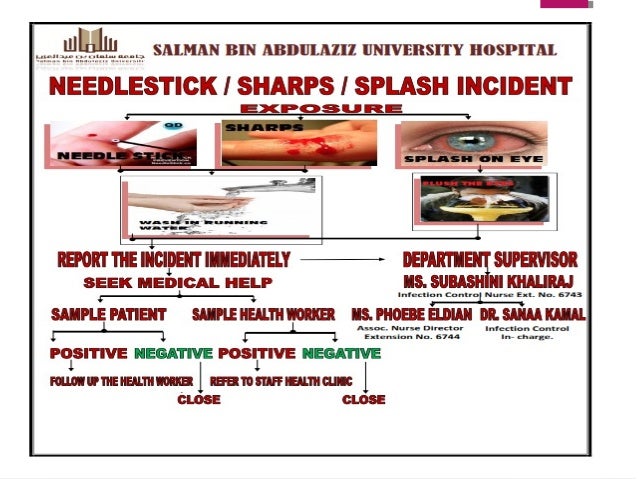
Medical students are at a particularly high risk for needlestick injury and its consequences because of their relative inexperience and lack of disability insurance. The response rate was 88% (157/178). Over one third (55/157) of respondents suffered at least 1 needlestick injury. In more than half
Reducing Needlestick Injuries . In the EU, more than one million needlestick injuries occur every year.1 Every day, healthcare workers across Europe are at risk of serious infections as a result of needlestick injuries involving over 30 potentially dangerous pathogens, including hepatitis B, hepatitis C and HIV.2 The greatest danger of infection comes from procedures using hollow-bore needles
Health Unit, Ministry of Health from 1998-2005, needlestick injury is the major cause of injuries among the Ministry of Health personnel which contributes to a total of 74.9 % of all injuries. Among the personnel, nurses
Needlestick injuries in the community are a source of great concern for parents. There is one reported case of seroconversion of Hepatitis B in children. The actual chance of viral transmission is very low.
Most needlestick injuries result from unsafe needle devices rather than carelessness by healthcare workers (JSHQ, 1998, Summer). Safer needle devices have built-in safety control devices, such as those that use a self-sheathing needle, to help prevent injuries before, during, and after use through safer design features.
The following are guidelines for what to do if you sustain a needlestick injury or body-fluid exposure. a) If the exposure occurs during working hours, care should be obtained from the Health Carousel Network contracted facility.
Following needlestick injury involving a known HIV-positive source, the one-year risk of seroconversion has been estimated to be 0.3%.5,6 In 1997, Cardo and colleagues identified four factors associated with increased risk for seroconversion after a needlestick/sharps injury from a known positive-HIV source:
Needlestick injury Wikipedia
Sharps and needlestick injuries Overview Special care should be taken during biological procedures to prevent injuries occurring while handling sharps such as needles, scalpels and stitch cutters.
Needlestick/Sharps Safety and Prevention The Needlestick Safety and Prevention Act (Pub. L. 106-430) was signed into law in November of 2000. Because occupational exposure to bloodborne pathogens from accidental sharps injuries in healthcare
Background. The risk of transmission of Blood Borne Viruses (BBV) to a needlestick recipient in a community setting is very low; There are no reported cases of a member of the public becoming infected by HIV, Hepatitis B or Hepatitis C following accidental injury from discarded injecting needles in the community setting
Needlestick injuries are wounds caused by needles that accidentally puncture the skin. Needlestick injuries are a hazard for people who work with hypodermic syringes and other needle equipment.
A needlestick injury is a piercing wound caused by a used and poten ally infected needle/syringe (or other used sharp such as a scalpel). These injuries are most common for workers handling needles in medical, dental, cleaning services and
Safety, Health and Wellbeing Needlestick/sharps injury and disposal of sharps guidelines. Our role is to develop and assist in the implementation of the UWA safety, health and wellbeing programs in order to minimise the risk of injury, illness and property damage.
Treating needlestick injuries. In Western Australia to date there has not been a documented case of a person contracting HIV, hepatitis B or hepatitis C from a needlestick injury that occurred in a community setting (such as a park or beach), and the risk is considered to be very low.
needlestick injury data including the personnel involved, the devices used, and the circumstances and frequency of needlestick events. This informa-tion can help in determining how employees can maximally benefit from a product change to safer needle devices. Although not required by OSHA, the collection and evaluation of complete needlestick injury data are key to identifying injury patterns
health care workers who contracted HIV from needlestick injuries involved injuries with hollow -bore, blood -filled needles ( CDC, 1998 a). This data may appear to be “old”, dating back five or six years. – analytical method validation protocol example Needle stick injury: A penetrating stab wound from a needle or syringe that may result in exposure to blood or other body fluids Sharps: Includes scissors, razors, lancets, scalpels, broken glassware,
Safety, Health and Wellbeing Needlestick injury. Our role is to develop and assist in the implementation of the UWA safety, health and wellbeing programs in order to minimise the risk of injury, illness and property damage.
toolkit-3-eMI Guidelines Appendices Appendix 1 Patient management form 28 Appendix 2 Flow chart for management of injuries 31 Appendix 3 Algorithm for needlestick/sharps exposure 32
Needlestick Injury Contents: Introduction p2 Reporting incidents p3 Protocol for management of exposures p15 Approaching source patients for blood-borne virus testing p16 Managing exposures from unknown sources p18 If the source patient is infected with HIV p19 If the source patient is infected with HCV p22 If the source patient is infected with HBV p22 If the source patient is unknown or
Category 4 injury (Needle stick injury that has progressed to necrosis or granulomatous ulceration). Perform surgical debridement to remove any residual vaccine material.
First aid. Contaminated needlestick, sharps injury, bite or scratch – encourage bleeding, wash with soap and running water. Blood or body fluid in the eyes or mouth – …
Needlestick Injury. Needlestick and sharps injuries are the most efficient method of transmitting bloodborne pathogens between patients and health care providers, and, therefore, they pose a significant risk to health care workers and students.
Must be used in conjunction with the NHSGGC guideline: Management of occupational and non-occupational exposures to bloodborne viruses MANAGEMENT OF NEEDLESTICK INJURIES AND
Page 1 of 22 The Newcastle upon Tyne Hospitals NHS Foundation Trust Policy for the Prevention and Management of Needlestick Injuries and Blood Borne Virus Exposures
a percutaneous injury (e.g., a needlestick or cut with a sharp object) or contact of mucous membrane or nonintact skin (e.g., exposed skin that is chapped, abraded, or afflicted with dermatitis) with blood, tissue, or other body fluids that are potentially infectious ( 16,17).
needlestick /sharps injuries and exposure to body fluids Director of Infection Prevention and Control (DIPC) – The DIPC is responsible for ensuring that HHFT has strategies to prevent avoidable HCAIs.
Needlestick Injuries in Dentistry ABSTRACT Needlestick injuries and other sharps-related injuries which expose health care professionals to bloodborne pathogens continue to be an important public health concern. Dentists are at increased risk of exposure to bloodborne pathogens, including Hepatitis B, Hepatitis C, and HIV. This article presents comprehensive information on Needlestick injuries
Needlestick – Injury The Safety Business Ltd www.safetybusiness.co.uk T 02076375047 Prevention… What to do… Never Always •Resheath needles •Over fill a sharps bin
MANAGING A NEEDLESTICK INJURY Stay calm > Allow the wound to bleed freely > Immediately wash the area with running water and soap, rinse and pat dry
CDC Emergency Needlestick Information
• a percutaneous injury (for example a needlestick or cut with sharp object); or • contact of mucous membranes or non-intact skin with blood, tissue or other bodily fluids that are potentially infectious.
Needlestick Protocol: WHAT TO DO If you are exposed to a needle stick, splash in the eye, or other high-risk exposure: 1. Immediately dispose of sharps safely, if necessary. 2. Explain to the patient that you will now transfer their care to another clinic worker, while you care for your injury, and ask them to wait for this transfer. 3. Notify your replacement clinic worker that you are
Emergency Sharps Information Workers Please Note. If you experienced a needlestick or sharps injury or were exposed to the blood or other body fluid of a patient during the course of your work, immediately follow these steps:
Only the highest risk needlestick injuries are offered HIV post-exposure prophylaxis which consists of 2-3 anti-retroviral medications administered for 28 days. For these scenarios, consult with the Infectious Diseases fellow during hours or consultant through switchboard after hours to discuss.
PDF Needlestick/Sharps Safety and Prevention NAU

Needlestick Injury World Gastroenterology Organisation
NEEDLESTICK INJURIES A Great Risk AWACC
Needlestick injury Safety Health and Wellbeing The
Needlestick Safety and Prevention who.int


Needlestick Injury – The Safety Business
https://lookformedical.com/en/wikipedia/needlestick-injuries
What Should I Do If I Get a Needlestick? The Hospitalist
ios custom delegate protocol example – Sharps Surveillance moh.gov.my
HC Needlestick Policy Tailored Healthcare Staffing
43. Guidelines on Needle stick Injury ODNS
Prevention and Management of Needlestick-Sharps Injuries
Needlestick/sharps injury and disposal of sharps
OSHA eTools Needlestick/Sharps Injuries
needlestick and other occupational injuries, especially in the light of recent legislative change (Human Tissue Act 2004 [HTA] and Mental Capacity Act 2005 [MCA]), and the withdrawal of previous guidance from the General Medical Council (GMC).
This guideline pertains to needlestick injuries from discarded needles in the community, usually from an unknown source where the risks of blood-borne virus (BBV) transmission, i.e. Hepatitis B, Hepatitis C and HIV, are very low.
The following are guidelines for what to do if you sustain a needlestick injury or body-fluid exposure. a) If the exposure occurs during working hours, care should be obtained from the Health Carousel Network contracted facility.
MANAGING A NEEDLESTICK INJURY Stay calm > Allow the wound to bleed freely > Immediately wash the area with running water and soap, rinse and pat dry
Needlestick injuries in the community are a source of great concern for parents. There is one reported case of seroconversion of Hepatitis B in children. The actual chance of viral transmission is very low.
Must be used in conjunction with the NHSGGC guideline: Management of occupational and non-occupational exposures to bloodborne viruses MANAGEMENT OF NEEDLESTICK INJURIES AND
A needlestick or sharps injury is said to have occurred if a staff member punctures the skin with a needle or sharp instrument that has been in contact with a patient’s blood. Splashing of the conjunctiva with blood or other body fluids is also included.
Needlestick injuries are a potential risk to health professionals who use needles and syringes in their clinical work. The New Zealand Health Strategy includes a framework and action plan to reduce the incidence and impact of infectious disease in an occupational setting. 1 Needlestick prevention protocols are an important element of the action
Needlestick – Injury The Safety Business Ltd www.safetybusiness.co.uk T 02076375047 Prevention… What to do… Never Always •Resheath needles •Over fill a sharps bin
ODNS 2015 89 43. Guidelines on Needle stick Injury The following information is abstracted from the South African Department of Health guidelines entitled:
Following needlestick injury involving a known HIV-positive source, the one-year risk of seroconversion has been estimated to be 0.3%.5,6 In 1997, Cardo and colleagues identified four factors associated with increased risk for seroconversion after a needlestick/sharps injury from a known positive-HIV source:
Needlestick Protocol: WHAT TO DO If you are exposed to a needle stick, splash in the eye, or other high-risk exposure: 1. Immediately dispose of sharps safely, if necessary. 2. Explain to the patient that you will now transfer their care to another clinic worker, while you care for your injury, and ask them to wait for this transfer. 3. Notify your replacement clinic worker that you are
Needlestick Injury. Needlestick and sharps injuries are the most efficient method of transmitting bloodborne pathogens between patients and health care providers, and, therefore, they pose a significant risk to health care workers and students.
REPORT ON THE INFECTION CONTROL PROTOCOL FOR NEEDLESTICK
NEEDLESTICK INJURIES POLICY University of Cape Town
toolkit-3-eMI Guidelines Appendices Appendix 1 Patient management form 28 Appendix 2 Flow chart for management of injuries 31 Appendix 3 Algorithm for needlestick/sharps exposure 32
Only the highest risk needlestick injuries are offered HIV post-exposure prophylaxis which consists of 2-3 anti-retroviral medications administered for 28 days. For these scenarios, consult with the Infectious Diseases fellow during hours or consultant through switchboard after hours to discuss.
Needlestick Protocol: WHAT TO DO If you are exposed to a needle stick, splash in the eye, or other high-risk exposure: 1. Immediately dispose of sharps safely, if necessary. 2. Explain to the patient that you will now transfer their care to another clinic worker, while you care for your injury, and ask them to wait for this transfer. 3. Notify your replacement clinic worker that you are
A needlestick injury, percutaneous injury, or percutaneous exposure incident or sharps injury is the penetration of the skin by a needle or other sharp object, which has been in contact with blood, tissue or other body fluids before the exposure.
from a Needle Stick Needle stick injuries pose a risk if the needle is contaminated with Hepatitis B, Hepatitis C or HIV virus. The risk of contracting an occupational disease caused by a needle stick depends on a number of factors: • the depth of penetration of the needle, • the amount of contaminated blood on the needle • when the needle was used, • the health status of the infected
Emergency Sharps Information Workers Please Note. If you experienced a needlestick or sharps injury or were exposed to the blood or other body fluid of a patient during the course of your work, immediately follow these steps:
Must be used in conjunction with the NHSGGC guideline: Management of occupational and non-occupational exposures to bloodborne viruses MANAGEMENT OF NEEDLESTICK INJURIES AND
A needlestick or sharps injury is said to have occurred if a staff member punctures the skin with a needle or sharp instrument that has been in contact with a patient’s blood. Splashing of the conjunctiva with blood or other body fluids is also included.
Following needlestick injury involving a known HIV-positive source, the one-year risk of seroconversion has been estimated to be 0.3%.5,6 In 1997, Cardo and colleagues identified four factors associated with increased risk for seroconversion after a needlestick/sharps injury from a known positive-HIV source:
Needlestick injuries are wounds caused by needles that accidentally puncture the skin. Needlestick injuries are a hazard for people who work with hypodermic syringes and other needle equipment.
CDC Emergency Needlestick Information
Sharps and needlestick injuries University of Technology
The AIDS Institute’s Office of the Medical Director needlestick injury procedure is as follows: If there is a needlestick injury and assistance is needed from the AIDS Institute,
MANAGING A NEEDLESTICK INJURY Stay calm > Allow the wound to bleed freely > Immediately wash the area with running water and soap, rinse and pat dry
toolkit-3-eMI Guidelines Appendices Appendix 1 Patient management form 28 Appendix 2 Flow chart for management of injuries 31 Appendix 3 Algorithm for needlestick/sharps exposure 32
Needlestick Injury Contents: Introduction p2 Reporting incidents p3 Protocol for management of exposures p15 Approaching source patients for blood-borne virus testing p16 Managing exposures from unknown sources p18 If the source patient is infected with HIV p19 If the source patient is infected with HCV p22 If the source patient is infected with HBV p22 If the source patient is unknown or
Needlestick/Sharps Safety and Prevention The Needlestick Safety and Prevention Act (Pub. L. 106-430) was signed into law in November of 2000. Because occupational exposure to bloodborne pathogens from accidental sharps injuries in healthcare
Page 1 of 22 The Newcastle upon Tyne Hospitals NHS Foundation Trust Policy for the Prevention and Management of Needlestick Injuries and Blood Borne Virus Exposures
The following are guidelines for what to do if you sustain a needlestick injury or body-fluid exposure. a) If the exposure occurs during working hours, care should be obtained from the Health Carousel Network contracted facility.
Category 4 injury (Needle stick injury that has progressed to necrosis or granulomatous ulceration). Perform surgical debridement to remove any residual vaccine material.
Health Unit, Ministry of Health from 1998-2005, needlestick injury is the major cause of injuries among the Ministry of Health personnel which contributes to a total of 74.9 % of all injuries. Among the personnel, nurses
Reducing Needlestick Injuries . In the EU, more than one million needlestick injuries occur every year.1 Every day, healthcare workers across Europe are at risk of serious infections as a result of needlestick injuries involving over 30 potentially dangerous pathogens, including hepatitis B, hepatitis C and HIV.2 The greatest danger of infection comes from procedures using hollow-bore needles
Needlestick Injury – from the community Page 2 of 4 Emergency Department Guideline Calculated from column 1 and 2. Maximal risk is likely overestimated.
ODNS 2015 89 43. Guidelines on Needle stick Injury The following information is abstracted from the South African Department of Health guidelines entitled:
Needlestick injuries in the community are a source of great concern for parents. There is one reported case of seroconversion of Hepatitis B in children. The actual chance of viral transmission is very low.
needlestick injury data including the personnel involved, the devices used, and the circumstances and frequency of needlestick events. This informa-tion can help in determining how employees can maximally benefit from a product change to safer needle devices. Although not required by OSHA, the collection and evaluation of complete needlestick injury data are key to identifying injury patterns
Sharps Surveillance moh.gov.my
MANAGEMENT OF NEEDLESTICK INJURIES AND EXPOSURES TO
Needlestick Injury: the accidental puncture of the skin by a needle during a medical intervention. Accidental exposure to blood: the unintended contact with blood and or with body fluids mixed with blood during a medical intervention.
needlestick injury data including the personnel involved, the devices used, and the circumstances and frequency of needlestick events. This informa-tion can help in determining how employees can maximally benefit from a product change to safer needle devices. Although not required by OSHA, the collection and evaluation of complete needlestick injury data are key to identifying injury patterns
First aid. Contaminated needlestick, sharps injury, bite or scratch – encourage bleeding, wash with soap and running water. Blood or body fluid in the eyes or mouth – …
needlestick /sharps injuries and exposure to body fluids Director of Infection Prevention and Control (DIPC) – The DIPC is responsible for ensuring that HHFT has strategies to prevent avoidable HCAIs.
An occupational exposure by an employee is defined as a needle stick, sharp puncture wound or a splash to mucous membranes (i.e., mouth or eye) with blood or body fluids as a result of an assignment at an affiliated hospital.
A needlestick or sharps injury is said to have occurred if a staff member punctures the skin with a needle or sharp instrument that has been in contact with a patient’s blood. Splashing of the conjunctiva with blood or other body fluids is also included.
Needlestick Injury. Needlestick and sharps injuries are the most efficient method of transmitting bloodborne pathogens between patients and health care providers, and, therefore, they pose a significant risk to health care workers and students.
needlestick injuries. LLÞtgog Queensland Health Centre for Healthcare Related Infection Surveillance and Prevention rnl/cc . Title: Poster: Protect Yourself and Others Author: CHRISP Subject: Five simple steps to avoid needlestick injuries Keywords: poster, needlestick injury, avoid needlestick Created Date : 8/9/2010 1:10:57 PM
Needle-stick injuries in members of the public A major source of distress is the needle-stick injury sustained by members of the community – usually from syringe/needle combinations that have been discarded in a public place.
for 63% of the needlestick injuries from June 1995 July 1999 (NIOSH, 1999). Ninety percent of the Centers for Disease Control and Prevention (CDC) document- ed cases of health care workers who contracted HIV from needlestick injuries
This guideline pertains to needlestick injuries from discarded needles in the community, usually from an unknown source where the risks of blood-borne virus (BBV) transmission, i.e. Hepatitis B, Hepatitis C and HIV, are very low.
POLICY & PROCEDURE SAFE HANDLING OF SHARPS & NEEDLE
Needlestick Injury World Gastroenterology Organisation
A needlestick injury means the skin is accidentally punctured by a used needle. Diseases that could be transmitted by a needle or needlestick injury include human immunodeficiency virus (HIV), hepatitis B and hepatitis C.
1 Recommendations on the Management and Postexposure Prophylaxis of Needlestick Injury or Mucosal Contact to HBV, HCV and HIV Background Occupational exposure …
health care workers who contracted HIV from needlestick injuries involved injuries with hollow -bore, blood -filled needles ( CDC, 1998 a). This data may appear to be “old”, dating back five or six years.
Safety, Health and Wellbeing Needlestick/sharps injury and disposal of sharps guidelines. Our role is to develop and assist in the implementation of the UWA safety, health and wellbeing programs in order to minimise the risk of injury, illness and property damage.
Needlestick Injury Contents: Introduction p2 Reporting incidents p3 Protocol for management of exposures p15 Approaching source patients for blood-borne virus testing p16 Managing exposures from unknown sources p18 If the source patient is infected with HIV p19 If the source patient is infected with HCV p22 If the source patient is infected with HBV p22 If the source patient is unknown or
needlestick injuries. LLÞtgog Queensland Health Centre for Healthcare Related Infection Surveillance and Prevention rnl/cc . Title: Poster: Protect Yourself and Others Author: CHRISP Subject: Five simple steps to avoid needlestick injuries Keywords: poster, needlestick injury, avoid needlestick Created Date : 8/9/2010 1:10:57 PM
Needle-stick injury (NSI) is a major occupational health and safety issue faced by healthcare professionals globally. This study was aimed to assess the frequency and factors associated with NSIs
Page 1 of 22 The Newcastle upon Tyne Hospitals NHS Foundation Trust Policy for the Prevention and Management of Needlestick Injuries and Blood Borne Virus Exposures
Category 4 injury (Needle stick injury that has progressed to necrosis or granulomatous ulceration). Perform surgical debridement to remove any residual vaccine material.
The AIDS Institute’s Office of the Medical Director needlestick injury procedure is as follows: If there is a needlestick injury and assistance is needed from the AIDS Institute,
Emergency Sharps Information Workers Please Note. If you experienced a needlestick or sharps injury or were exposed to the blood or other body fluid of a patient during the course of your work, immediately follow these steps:
Needle stick injury: A penetrating stab wound from a needle or syringe that may result in exposure to blood or other body fluids Sharps: Includes scissors, razors, lancets, scalpels, broken glassware,
Needlestick injuries in the community are a source of great concern for parents. There is one reported case of seroconversion of Hepatitis B in children. The actual chance of viral transmission is very low.
Following needlestick injury involving a known HIV-positive source, the one-year risk of seroconversion has been estimated to be 0.3%.5,6 In 1997, Cardo and colleagues identified four factors associated with increased risk for seroconversion after a needlestick/sharps injury from a known positive-HIV source:
precaution guidelines and Malaysia infection control guidelines with objectives to promote the students interests on the universal precaution measures on needle sticks injury and to prevent future transmission of infection through needle stick injuries. So we had set the objectives for the research to study the effectiveness of Needle stick injury prevention intervention model on accidental
Needlestick Protocol PDF documents – Docucu-Archive.com
Needlestick injury Better Health Channel
Treating needlestick injuries. In Western Australia to date there has not been a documented case of a person contracting HIV, hepatitis B or hepatitis C from a needlestick injury that occurred in a community setting (such as a park or beach), and the risk is considered to be very low.
needlestick and other occupational injuries, especially in the light of recent legislative change (Human Tissue Act 2004 [HTA] and Mental Capacity Act 2005 [MCA]), and the withdrawal of previous guidance from the General Medical Council (GMC).
Safety, Health and Wellbeing Needlestick/sharps injury and disposal of sharps guidelines. Our role is to develop and assist in the implementation of the UWA safety, health and wellbeing programs in order to minimise the risk of injury, illness and property damage.
Health Unit, Ministry of Health from 1998-2005, needlestick injury is the major cause of injuries among the Ministry of Health personnel which contributes to a total of 74.9 % of all injuries. Among the personnel, nurses
NEEDLE STICK INJURIES Sharps injuries are the most frequent occupational hazard faced by nurses, phlebotomists, doctors and other healthcare workers1.
Needlestick Injury – from the community Page 2 of 4 Emergency Department Guideline Calculated from column 1 and 2. Maximal risk is likely overestimated.
Only the highest risk needlestick injuries are offered HIV post-exposure prophylaxis which consists of 2-3 anti-retroviral medications administered for 28 days. For these scenarios, consult with the Infectious Diseases fellow during hours or consultant through switchboard after hours to discuss.
Needlestick injuries in the community are a source of great concern for parents. There is one reported case of seroconversion of Hepatitis B in children. The actual chance of viral transmission is very low.
Treating needlestick injuries Healthy WA
(PDF) Needle-stick injury A rising bio-hazard ResearchGate
precaution guidelines and Malaysia infection control guidelines with objectives to promote the students interests on the universal precaution measures on needle sticks injury and to prevent future transmission of infection through needle stick injuries. So we had set the objectives for the research to study the effectiveness of Needle stick injury prevention intervention model on accidental
OSHA eTools Needlestick/Sharps Injuries
Needle Stick Injuries Protecting Workers in the Municipal
REPORT ON THE INFECTION CONTROL PROTOCOL FOR NEEDLESTICK
An occupational exposure by an employee is defined as a needle stick, sharp puncture wound or a splash to mucous membranes (i.e., mouth or eye) with blood or body fluids as a result of an assignment at an affiliated hospital.
MANAGING A NEEDLESTICK INJURY sahealth.sa.gov.au
Needlestick Protocol PDF documents – Docucu-Archive.com
Needlestick and Sharps Injuries OSH Answers
Needle stick injury: A penetrating stab wound from a needle or syringe that may result in exposure to blood or other body fluids Sharps: Includes scissors, razors, lancets, scalpels, broken glassware,
Needle Stick Injuries Protecting Workers in the Municipal
1 Recommendations on the Management and Postexposure Prophylaxis of Needlestick Injury or Mucosal Contact to HBV, HCV and HIV Background Occupational exposure …
Sharps and needlestick injuries University of Technology
NEEDLESTICK INJURIES POLICY University of Cape Town
Category 4 injury (Needle stick injury that has progressed to necrosis or granulomatous ulceration). Perform surgical debridement to remove any residual vaccine material.
St Gemma’s Hospice INFECTION CONTROL NEEDLESTICK OR
Needle Stick Protocol dentaltown.com
Needlestick Injury: the accidental puncture of the skin by a needle during a medical intervention. Accidental exposure to blood: the unintended contact with blood and or with body fluids mixed with blood during a medical intervention.
Sharps Injuries Prevention in the NSW Public Health
MANAGEMENT OF NEEDLESTICK INJURIES AND EXPOSURES TO
Needlestick injuries are wounds caused by needles that accidentally puncture the skin. Needlestick injuries are a hazard for people who work with hypodermic syringes and other needle equipment.
43. Guidelines on Needle stick Injury ODNS
Safety, Health and Wellbeing Needlestick injury. Our role is to develop and assist in the implementation of the UWA safety, health and wellbeing programs in order to minimise the risk of injury, illness and property damage.
Association of Anaesthetists of Great Britain & Ireland
A needlestick injury means the skin is accidentally punctured by a used needle. Diseases that could be transmitted by a needle or needlestick injury include human immunodeficiency virus …
Sharps and needlestick injuries University of Technology
ODNS 2015 89 43. Guidelines on Needle stick Injury The following information is abstracted from the South African Department of Health guidelines entitled:
MANAGEMENT OF NEEDLESTICK INJURIES AND EXPOSURES TO
In this section. Australian National Guidelines for the Management of Healthcare Workers Living with Blood Borne Viruses and Healthcare Workers who Perform Exposure Prone Procedures at Risk of Exposure to Blood Borne Viruses
BRIEF REPORT Needlestick Injury and Inadequate Post
Needlestick Injury Procedure
Department of Health Australian National Guidelines for
a percutaneous injury (e.g., a needlestick or cut with a sharp object) or contact of mucous membrane or nonintact skin (e.g., exposed skin that is chapped, abraded, or afflicted with dermatitis) with blood, tissue, or other body fluids that are potentially infectious ( 16,17).
NHS Needlestick Injury pdf nhsemployers.org
Recommendations on the postexposure Management and
Needlestick Injury from the community – Kids Health WA
A needlestick injury means the skin is accidentally punctured by a used needle. Diseases that could be transmitted by a needle or needlestick injury include human immunodeficiency virus (HIV), hepatitis B and hepatitis C.
Needlestick Injuries in Dentistry KUMJ
MANAGEMENT OF NEEDLESTICK INJURIES AND EXPOSURES TO
Sharps and needlestick injuries University of Technology
A needlestick injury means the skin is accidentally punctured by a used needle. Diseases that could be transmitted by a needle or needlestick injury include human immunodeficiency virus …
Needlestick injuries in a healthcare setting in New
BRIEF REPORT Needlestick Injury and Inadequate Post
NEEDLESTICK INJURIES POLICY Policy for the procedures to follow in the event of staff and students who have been exposed to blood and blood stained body fluids in the course of carrying out their duties.
Needle-Stick Policy
Needle-stick injury (NSI) is a major occupational health and safety issue faced by healthcare professionals globally. This study was aimed to assess the frequency and factors associated with NSIs
CAUT Health and Safety Fact Sheet
Medical students are at a particularly high risk for needlestick injury and its consequences because of their relative inexperience and lack of disability insurance. The response rate was 88% (157/178). Over one third (55/157) of respondents suffered at least 1 needlestick injury. In more than half
BRIEF REPORT Needlestick Injury and Inadequate Post
MANAGING A NEEDLESTICK INJURY sahealth.sa.gov.au
NEEDLESTICK INJURIES A Great Risk AWACC
Needlestick Injuries in Dentistry ABSTRACT Needlestick injuries and other sharps-related injuries which expose health care professionals to bloodborne pathogens continue to be an important public health concern. Dentists are at increased risk of exposure to bloodborne pathogens, including Hepatitis B, Hepatitis C, and HIV. This article presents comprehensive information on Needlestick injuries
POLICY & PROCEDURE SAFE HANDLING OF SHARPS & NEEDLE
Management of healthcare workers after occupational
Management of Occupational Exposures to HBV HCV and HIV
Needlestick Injury Contents: Introduction p2 Reporting incidents p3 Protocol for management of exposures p15 Approaching source patients for blood-borne virus testing p16 Managing exposures from unknown sources p18 If the source patient is infected with HIV p19 If the source patient is infected with HCV p22 If the source patient is infected with HBV p22 If the source patient is unknown or
Prevention and Management of Needlestick-Sharps Injuries
Needlestick Injury. Understanding needlestick injuries
Clearly, the appropriate management of needlestick injuries poses a new challenge to the healthcare sector, both in terms of reducing the overall risk of needlestick injury, the fair and reasonable management of injured staff and the protection of patients.
Needlestick Injury. Understanding needlestick injuries
Needlestick Injury – The Safety Business
Treating needlestick injuries Healthy WA
A needlestick injury, percutaneous injury, or percutaneous exposure incident or sharps injury is the penetration of the skin by a needle or other sharp object, which has been in contact with blood, tissue or other body fluids before the exposure.
Sharps Surveillance moh.gov.my
Needlestick Injury World Gastroenterology Organisation
The purpose of this report is to present the Infection Control Protocol for Needlestick and Similar Sharps Injuries for approval. The Protocol is attached
OSHA eTools Needlestick/Sharps Injuries
Community needle stick injury Children’s Health Queensland
Needlestick injury Wikipedia
NEEDLE STICK INJURIES Sharps injuries are the most frequent occupational hazard faced by nurses, phlebotomists, doctors and other healthcare workers1.
Needlestick Injury Procedure
Management of community needle stick injury (CNSI): Presentations of children to Emergency Departments following accidental needle stick injury are not uncommon and such injuries may be a significant source of anxiety.
Recommendations on the postexposure Management and
needlestick injury data including the personnel involved, the devices used, and the circumstances and frequency of needlestick events. This informa-tion can help in determining how employees can maximally benefit from a product change to safer needle devices. Although not required by OSHA, the collection and evaluation of complete needlestick injury data are key to identifying injury patterns
REPORT ON THE INFECTION CONTROL PROTOCOL FOR NEEDLESTICK
Needle-stick injury (NSI) is a major occupational health and safety issue faced by healthcare professionals globally. This study was aimed to assess the frequency and factors associated with NSIs
Sharps Injuries Prevention in the NSW Public Health
Treating needlestick injuries Healthy WA
POLICY & PROCEDURE SAFE HANDLING OF SHARPS & NEEDLE
The following are guidelines for what to do if you sustain a needlestick injury or body-fluid exposure. a) If the exposure occurs during working hours, care should be obtained from the Health Carousel Network contracted facility.
Poster Protect Yourself and Others Queensland Health
Only the highest risk needlestick injuries are offered HIV post-exposure prophylaxis which consists of 2-3 anti-retroviral medications administered for 28 days. For these scenarios, consult with the Infectious Diseases fellow during hours or consultant through switchboard after hours to discuss.
Needlestick Injury World Gastroenterology Organisation
•the safety feature cannot be deactivated and remains protective through disposal Workplace Protocol •Use the devices with safety fea-tures provided by the employer.
Recommendations on the postexposure Management and
Needlestick Injuries in Dentistry KUMJ
CAUT Health and Safety Fact Sheet
Needlestick injuries are wounds caused by needles that accidentally puncture the skin. Needlestick injuries are a hazard for people who work with hypodermic syringes and other needle equipment.
Needlestick Injury Procedure
Management of healthcare workers after occupational
Terumo Needlestick prevention Australian Hospital
Page 1 of 22 The Newcastle upon Tyne Hospitals NHS Foundation Trust Policy for the Prevention and Management of Needlestick Injuries and Blood Borne Virus Exposures
MANAGEMENT OF NEEDLESTICK INJURIES AND EXPOSURES TO
Poster Protect Yourself and Others Queensland Health
Management of healthcare workers after occupational
Needlestick and sharps injuries are recognised as one of the significant occupational hazards faced by healthcare workers every day. Every needlestick or sharps injury carries the risk of acquiring a potentially life threatening bloodborne disease such as hepatitis B or C, or HIV/AIDS.
TITLE Farmer Needlestick Injuries Risk & TYPE
for 63% of the needlestick injuries from June 1995 July 1999 (NIOSH, 1999). Ninety percent of the Centers for Disease Control and Prevention (CDC) document- ed cases of health care workers who contracted HIV from needlestick injuries
Needlestick Injury from the community – Kids Health WA
Management of healthcare workers after occupational
Policy for the prevention and management of Needlestick
Needlestick – Injury The Safety Business Ltd http://www.safetybusiness.co.uk T 02076375047 Prevention… What to do… Never Always •Resheath needles •Over fill a sharps bin
REPORT ON THE INFECTION CONTROL PROTOCOL FOR NEEDLESTICK
Knowledge Attitude and Practices about Needle Stick
A needlestick injury is a piercing wound caused by a used and poten ally infected needle/syringe (or other used sharp such as a scalpel). These injuries are most common for workers handling needles in medical, dental, cleaning services and
Fact Sheet Needlestick injury by Better Health Channel
43. Guidelines on Needle stick Injury ODNS
Needlestick/sharps injury and disposal of sharps
Only the highest risk needlestick injuries are offered HIV post-exposure prophylaxis which consists of 2-3 anti-retroviral medications administered for 28 days. For these scenarios, consult with the Infectious Diseases fellow during hours or consultant through switchboard after hours to discuss.
Needlestick injuries in a healthcare setting in New
Needlestick injuries are wounds caused by needles that accidentally puncture the skin. Needlestick injuries are a hazard for people who work with hypodermic syringes and other needle equipment.
Needlestick Injury – from the community
Needlestick injuries in a healthcare setting in New
Department of Health Australian National Guidelines for
A needlestick or sharps injury is said to have occurred if a staff member punctures the skin with a needle or sharp instrument that has been in contact with a patient’s blood. Splashing of the conjunctiva with blood or other body fluids is also included.
Needlestick Injury World Gastroenterology Organisation
BRIEF REPORT Needlestick Injury and Inadequate Post
Needlestick injuries are wounds caused by needles that accidentally puncture the skin. Needlestick injuries are a hazard for people who work with hypodermic syringes and other needle equipment.
Needlestick Injury. Understanding needlestick injuries
Needlestick Injuries in Dentistry ABSTRACT Needlestick injuries and other sharps-related injuries which expose health care professionals to bloodborne pathogens continue to be an important public health concern. Dentists are at increased risk of exposure to bloodborne pathogens, including Hepatitis B, Hepatitis C, and HIV. This article presents comprehensive information on Needlestick injuries
Association of Anaesthetists of Great Britain & Ireland
Needle-stick injuries in primary care Australian Prescriber
needlestick and other occupational injuries, especially in the light of recent legislative change (Human Tissue Act 2004 [HTA] and Mental Capacity Act 2005 [MCA]), and the withdrawal of previous guidance from the General Medical Council (GMC).
Clinical Practice Guidelines Needle stick injury
Page 1 of 22 The Newcastle upon Tyne Hospitals NHS Foundation Trust Policy for the Prevention and Management of Needlestick Injuries and Blood Borne Virus Exposures
Needlestick Injury Procedure
Terumo Needlestick prevention Australian Hospital
• a percutaneous injury (for example a needlestick or cut with sharp object); or • contact of mucous membranes or non-intact skin with blood, tissue or other bodily fluids that are potentially infectious.
Needlestick Injuries in Dentistry KUMJ
Health Unit, Ministry of Health from 1998-2005, needlestick injury is the major cause of injuries among the Ministry of Health personnel which contributes to a total of 74.9 % of all injuries. Among the personnel, nurses
Needle-Stick Policy
This guideline pertains to needlestick injuries from discarded needles in the community, usually from an unknown source where the risks of blood-borne virus (BBV) transmission, i.e. Hepatitis B, Hepatitis C and HIV, are very low.
PDF Needlestick/Sharps Safety and Prevention NAU
POLICY & PROCEDURE SAFE HANDLING OF SHARPS & NEEDLE
American Nurses Association’s Needlestick Prevention Guide
The AIDS Institute’s Office of the Medical Director needlestick injury procedure is as follows: If there is a needlestick injury and assistance is needed from the AIDS Institute,
Terumo Needlestick prevention Australian Hospital
NEEDLESTICK INJURIES POLICY Policy for the procedures to follow in the event of staff and students who have been exposed to blood and blood stained body fluids in the course of carrying out their duties.
Prevention and Management of Needlestick-Sharps Injuries
Here are some other needlestick resources from http://www.drotterholt.com. [Editor’s note: Visit Dentaltown.com to view these links.] Post-Exposure Prophylaxis Hotline (PEPline) is a national toll-free hotline (24 hours a day)
Policy for the prevention and management of Needlestick
Needlestick Protocol PDF documents – Docucu-Archive.com
Following needlestick injury involving a known HIV-positive source, the one-year risk of seroconversion has been estimated to be 0.3%.5,6 In 1997, Cardo and colleagues identified four factors associated with increased risk for seroconversion after a needlestick/sharps injury from a known positive-HIV source:
(PDF) Needle-stick injury A rising bio-hazard ResearchGate